Health Talk Blog
NOVEMBER BLOG
LIVING WITH COPD
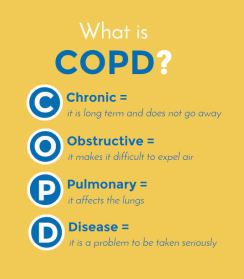
What Is COPD?
Chronic obstructive pulmonary disease or COPD, is actually two long-term lung diseases -- chronic bronchitis and emphysema. They often times occur together. It all boils down to - COPD makes it hard for you to breathe!
Within the lung structure, there are airways, or tubing, that carry air into and out of your lungs. With COPD, the airways sometimes become partly blocked from swelling or mucus, making it hard to breathe.
At the end of the airways are tiny air sacs, small balloons that inflate and deflate when you breathe in and out. With COPD, these sacs become less flexible when breathing. This can cause small airways to cave in or collapse, making it harder to breathe.
What Causes COPD?
- Smoking. 80 to 90% of most cases of COPD are caused by smoking, but you don’t have to be a smoker to get it. You can also get it from tobacco products, such as cigar and pipe smoke, especially if you breathe in the smoke. Secondhand smoke is also an issue.
- Pollution and fumes. Breathing in chemical fumes, dust or toxic substances at work can also cause it.
- Your genes. In rare cases, people with COPD have a defect in their DNA, the code that tells your body how to work properly. The defect - alpha-1 antitrypsin deficiency, or AAT, lungs don't have enough of a protein needed to protect them from damage. If you or a family member had serious lung problems -- especially at a young age -- ask your doctor about testing for AAT deficiency.
- Asthma. If not treated asthma, over time will produce lifetime damage to the lungs.
Signs & Symptoms of COPD - COPD is a progressive disease which typically gets worse over time.
• Shortness of breath or "dyspnea": when you breathe harder but feel like you're running out of air
• Persistent (chronic) cough
• Coughing up mucus/phlegm
• Difficult or labored breathing during physical activity or while resting
• Wheezing (air trying to flow through a narrow airway)
• More frequent colds or flu
Other associated signs and symptoms:
• Fatigue/tiredness
• Weight loss
• Morning headaches - breathing decreases during sleep, decreasing oxygen levels while carbon dioxide levels build up in the blood causing headaches.
There may be times of occasional suddenly "flare up" or symptoms are worse than usual. The severe symptoms, or exacerbations, should be taken seriously. Many exacerbations are caused by a viral or bacterial lung infection.
When to Call a Doctor - The following symptoms usually mean there is an infection present. Make sure to talk with your healthcare provider if you're experiencing any of the COPD symptoms listed.
- Shortness of breath or coughing more than usual.
- Shortness of breath affects your daily routine.
- Coughing up more mucus than normal.
- The mucus has colors: yellow, green, or rust-colored.
- You have a fever over 101 F.
- You feel dizzy or lightheaded
Types of Tests for COPD
Your doctor may recommend several tests to get the right diagnosis. They might include:
- Spirometry. Tests the amount of air you can breathe in and out. You will be asked to take a deep breath and blow hard into a mouthpiece connected to a small machine, a spirometer.
- Chest X-ray. An image of the chest, including your heart, lungs and blood vessels.
- Chest CT scan. Also an image of the chest with more details than a chest X-ray. A dye may be injected into a vein to enable a clearer image of the chest.
- Arterial blood gas test. This test measures the amount of oxygen and carbon dioxide flowing in your bloodstream.
- Alpha-1 Antitrypsin Deficiency Testing. For a protein called AAT, found in your lungs and blood.
What Are the Stages of COPD? The level of severity in your diagnosis will dictate the level of treatment you will receive. Doctors use stages to describe COPD severity. This classification system is called the GOLD staging or grading system.
- How many times has your COPD has gotten worse
- Number of hospitalizations because your COPD has gotten worse
- Spirometry testing.
- GOLD 1: mild
- GOLD 2: moderate
- GOLD 3: severe
- GOLD 4: very severe
- Forced vital capacity, FVC – the largest amount of air breathed out after breathing in as deeply as you can.
- Forced expiratory volume, FEV-1 - how much air exhaled from your lungs in one second.
The doctor then assigns a grade to additional information:
- How severe your current symptoms are
- Your spirometry results
- The chances that your COPD will get worse
- The presence of other health problems
Symptom Grades - The assessments will consist of the COPD Assessment Test, CAT, or the Modified Medical Research Council, mMRC.
- CAT scores range from 0-40.
- mMRC scores range from hard exercise an MRA Grade 0 to severely breathless an mMRA Grade 4.
Who's on your healthcare team? Evaluate the people who play a role in your wellbeing who assist you to make and reach your COPD goals:
- Primary Care Provider (PCP) - a doctor, physician assistant, PA, or nurse practitioner, NP. Your PCP plays a key role in the diagnosis and management of COPD.
- Pulmonologist - specialize in diagnosing and treating people with lung conditions, like COPD.
- Pharmacist - prepares and processes prescription and may also follow your progress to ensure medications are appropriate for you and your medication plan
- Respiratory Therapist - work in hospitals or travel to patients' homes. They help patients manage home oxygen needs and how to manage their COPD condition.
- Nurse - the first point of contact for patients and involved in all stages of care
To Quit Smoking You Need a Good Support - Quitting smoking is one of the hardest things you can do! My mother started smoking at age 14. As she was diagnosed with emphysema, then COPD, then finally 4th stage lung cancer, she professed the inability to quit even with our cries to stop. It was hard watching her suffer with the disease as it progressed. You don’t have to do it alone! Our family was with her the entire time, taking shifts with her care – family support!
Developing healthy eating habits - Add more fruits and vegetables to your diet. Eating right provides more energy for all your daily activities, including breathing. Maintaining a healthy weight is important because the lungs work harder to breathe with COPD. Good nutrition also helps the body fight infections.
Sleep and Rest - Sleep and rest are significantly more important when living with COPD. A good night's sleep can provide energy for day-to-day activities.
- LOW OXYGEN LEVELS - You may or may not know if you have a low oxygen level when you sleep.
- SLEEP APNEA – or obstructive sleep, is a common disorder which causes you to stop breathing during sleep, from a few seconds, to a minute or longer, at least 3 nights a week.
- MEDICATIONS - Medications taken near bedtime may hamper the ability of falling asleep.
- COUGHING - wakes you up or interrupts sleep during the night.
Do's and don'ts for a good night's sleep
DO’S:
- Keep your room quiet, dark and cool.
- Develop a bedtime routine.
- Relax before bedtime.
- Try to go to sleep and wake up at the same time including weekends.
DON'T
- Get into bed until you are tired.
- Nap.
- Drink caffeine.
What medication can help improve symptoms of chronic obstructive pulmonary disease (COPD)?
Medications for COPD can help improve lung capacity, ease inflammation, relax muscles in the airway and improve breathing. They include:
- Bronchodilators - breathe in through an inhaler. These come in short- and long-acting forms. Some stop muscles in the airway from tightening up (anticholinergics). Others relax muscles already tight (beta agonists).
- Anti-inflammatory meds or corticosteroids, steroids, are often inhaled drugs for COPD. If symptoms get worse, you may take pills for a short time.
- Antibiotics - to fight infections that cause symptom flare-ups.
- Vaccinations - against flu or pneumonia.
- Roflumilast (Daliresp) - is the first of a new class of COPD drugs called phosphodiesterase-4 inhibitors that ease flares for people at the severe stage.
- Oxygen therapy - gives you more energy for daily tasks and helps with sleep.
- Surgery - can remove diseased lung tissue, make lungs smaller to breathe easier, or a lung transplant.
- Pulmonary rehabilitation - includes exercises and good nutrition to help improve breathing and overall health.
HERB AND SUPPLEMENT SUGGESTIONS
- Eucalyptus - The dried leaves and oil are used to make medicine. Some uses include - asthma, bronchitis, plaque and gingivitis, head lice, toe nail fungus and many others. Early research shows that eucalyptol, a chemical found in eucalyptus oil, may aid in breaking up mucous in people with asthma. Some people with severe asthma have been able to lower their dosage of steroid medications if they take eucalyptol. It may also block chemicals that cause asthma. Taking eucalyptus oil along with some medications that are broken down by the liver can increase the effects and side effects of some medications.
- Oregano Oil - Oregano is used for respiratory tract disorders such as coughs, asthma, croup and bronchitis. It is also used for gastrointestinal (GI) disorders such as heartburn and bloating. Oregano contains chemicals that might help reduce cough and spasms. Oregano might have an effect like a water pill or "diuretic.”
- Turmeric - is used in Ayurvedic medicine to treat inflammation -- both inside and out. A tablespoon of ground turmeric offers 29 calories, nearly a gram of protein, 2 grams of fiber and 6 grams of carbohydrates. It contains minerals such as manganese, phosphorus and potassium.
- Garlic - produces a chemical called allicin. This is what seems to make garlic work for certain conditions. Allicin also makes garlic smell. Garlic is used for many conditions related to the heart and blood system. It is also used to treat prostate cancer and bladder cancer.
- Ginger - Ginger contains chemicals that may reduce nausea and inflammation. Research suggests that administering 120 mg of ginger extract daily for up to 21 days increases the number of days without ventilator support, the amount of nutrients consumed, and reduces the time spent in intensive care units in people with sudden respiratory system a failure.
- Reishi mushrooms – have anti-inflammatory properties. The most important effect of the Reishi mushroom is their anti-inflammatory capacity. For healthy respirations,
those suffering from asthma, bronchitis or other chronic respiratory conditions, reishi mushrooms have a strong effect on reducing irritation and eliminating the allergic reactions from the body. By preventing the release of histamine from mast cells in the body, reishi mushrooms prevent allergic reactions, from mild skin irritation to potentially life-threatening anaphylaxis.
- Cordyceps - extract is seen to help maintain regular heart rhythms. Promisingly, a 2008 laboratory study showed that cordyceps extract helped to lower the rate of rejection of heart transplants in a laboratory rat model. Cordyceps is also helpful in maintaining lymphocyte (orchestrators of the immune system’s response to infections and injury) and macrophage function (a type of cell responsible for detecting, engulfing and destroying pathogens, damaged and dying cells in the body) within normal levels in laboratory results.
ALWAYS CONSULT YOUR PERSONAL HEALTH CARE PROFESSIONAL
- https://www.webmd.com/lung/copd/10-faqs-about-living-with-copd#1
- https://www.webmd.com/lung/copd/what-causes-copd#1
- https://www.webmd.com/lung/copd/what-are-symptoms-of-copd
- https://www.copd.com/copd-management/sleep-and-rest.html
- https://www.copd.com/copd-management/activities.html
- https://www.copd.com/copd-management/exercise.html
- https://www.copd.com/copd-management/pulmonary-rehabilitation.html
- https://www.copd.com/copd-management/copd-diet.html
- https://www.copd.com/copd-management/
- https://www.copd.com/copd-care-plan/quit-smoking.html
- https://www.copd.com/copd-care-plan/treatment.html
- https://www.copd.com/copd-care-plan/action-plan.html
- https://www.copd.com/copd-care-plan/
- https://www.copd.com/about-copd/exacerbations.html
- https://www.copd.com/about-copd/diagnosis.html
- https://www.copd.com/about-copd/symptoms.html
- https://www.webmd.com/vitamins/ai/ingredientmono-700/eucalyptus
- https://www.webmd.com/vitamins/ai/ingredientmono-644/oregano
- https://www.webmd.com/food-recipes/features/why-ls-turmeric-good-for-me
- https://www.webmd.com/vitamins/ai/ingredientmono-300/garlic
- https://www.webmd.com/vitamins/ai/ingredientmono-961/ginger
- https://www.webmd.com/vitamins/ai/ingredientmono-1500/fermented-wheat-germ-extract
- https://www.organicfacts.net/health-benefits/other/reishi-mushrooms.html
- https://organixx.com/cordyceps-mushroom/